The path to individualization of infusion therapy for emergency conditions according to the ROSE concept
 Abstract. The article is devoted to the role of intravenous fluid therapy in conditions of impaired fluid homeostasis, which often occur during major surgical interventions and critical conditions, such as sepsis and trauma. The importance of adequate fluid administration to maintain cellular homeostasis, as well as the management of conditions associated with hypovolemia and hemodynamic disturbances, is described. It is noted that, despite numerous studies, the topic of optimal fluid management strategies remains controversial, with potential risks of adverse effects of excessive fluid administration on clinical outcomes.
Abstract. The article is devoted to the role of intravenous fluid therapy in conditions of impaired fluid homeostasis, which often occur during major surgical interventions and critical conditions, such as sepsis and trauma. The importance of adequate fluid administration to maintain cellular homeostasis, as well as the management of conditions associated with hypovolemia and hemodynamic disturbances, is described. It is noted that, despite numerous studies, the topic of optimal fluid management strategies remains controversial, with potential risks of adverse effects of excessive fluid administration on clinical outcomes.
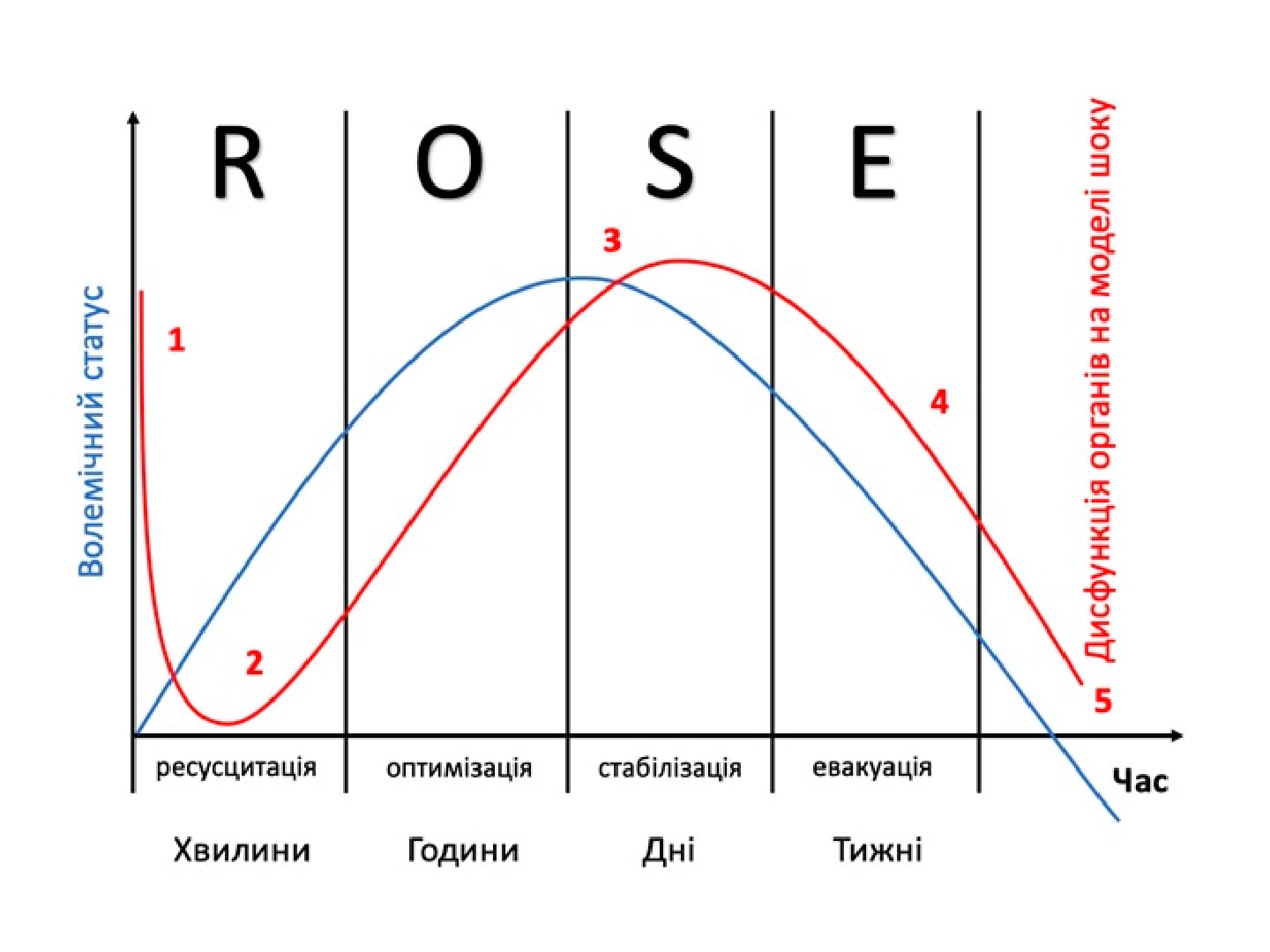
The concept of liquid resuscitation ROSE is presented, which includes four stages: resuscitation, optimization, stabilization and evacuation. This concept will assist physicians in making decisions about fluid therapy management. Different types of fluids are reviewed, including balanced solutions and the multifunctional hyperosmolar solution Reosorbilact, and the importance of individualizing therapy based on the needs of each patient is emphasized. The importance of the need for careful monitoring and control of fluid balance is emphasized to avoid complications and ensure improved clinical outcomes.
Keywords: infusion therapy, trauma, sepsis, emergency fluid resuscitation.
Authors:
- Dzyuba Dmytro Oleksandrovych1,2
- Nedashkivskyi Serhiy Mykhailovych1
1 KNP KOR “Kyiv Regional Clinical Hospital”.
2 Shupyk National Healthcare University of Ukraine, Kyiv.
Literature:
- Edwards, M. R., & Mythen, M. G. (2014). Fluid therapy in critical illness. Extreme Physiology & Medicine, 3, 1-9.
- Hoste, E. A. et al. (2014). Four phases of intravenous fluid therapy: a conceptual model. British Journal of Anaesthesia, 113(5), 740-747.
- Myburgh, J. A., & Mythen, M. G. (2013). Resuscitation Fluids. New England Journal of Medicine, 369, 1243–1251.
- Dellinger, R. P., Levy, M. M., Rhodes, A. et al. (2013). Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Critical Care Medicine, 41, 580−637.
- Marik, P. E., Monnet, X., & Teboul, J. L. (2011). Haemodynamic parameters to guide fluid therapy. Annals of Intensive Care, 1, 1.
- Chowdhury, A. H., Cox, E. F., Francis, S. T., & Lobo, D. N. (2012). A randomised, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and Plasmalyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Annals of Surgery, 256, 18−24.
- Sanchez, M., Jimenez-Lendinez, M., Cidoncha, M. et al. (2011). Comparison of fluid management in non-septic patients. Anaesthesia and Intensive Care, 39, 1022−1029.
- Malbrain, M. et al. (2014). Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anestezjologia Intensywna Terapia, 46(5), 377-396.
- Marik, P. E. (2014). Iatrogenic salt water drowning and the hazards of a high central venous pressure. Annals of Intensive Care, 4, 21.
- Malbrain, M., & Van Regenmortel, N. (2012). Fluid overload is not only of cosmetic concern (Part I): Exploring a new hypothesis. ICU Management, 12, 30−33.
- Messmer, A. S. et al. (2023). Active fluid de-resuscitation in critically ill patients with septic shock: A systematic review and meta-analysis. European Journal of Internal Medicine, 109, 89-96.
- Magder, S. (2016). Volume and its relationship to cardiac output and venous return. Critical Care, 20, 271.
- Miller, T. E., Roche, A. M., & Mythen, M. (2015). Fluid management and goal-directed therapy as an adjunct to Enhanced Recovery After Surgery (ERAS). Canadian Journal of Anaesthesia, 62(2), 158–168.
- Malbrain, M. L. N. G. et al. (2020). Intravenous fluid therapy in the perioperative and critical care setting: executive summary of the International Fluid Academy (IFA). Annals of Intensive Care, 10, 1-19.
- Acheampong, A., & Vincent, J. L. (2015). A positive fluid balance is an independent prognostic factor in patients with sepsis. Critical Care, 19, 251.
- De Oliveira, F. S. et al. (2015). Positive fluid balance as a prognostic factor for mortality and acute kidney injury in severe sepsis and septic shock. Journal of Critical Care, 30(1), 97–101.
- Silva, J. M. Jr et al. (2013). The effect of excess fluid balance on the mortality rate of surgical patients: a multicenter prospective study. Critical Care, 17(6), R288.
- Marik, P. E. et al. (2017). Fluid administration in severe sepsis and septic shock: patterns and outcomes: an analysis of a large national database. Intensive Care Medicine, 43(5), 625–632.
- Cordemans, C. et al. (2012). Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Annals of Intensive Care, 2(Suppl 1), S15.
- Vincent, J. L., & De Backer, D. (2013). Circulatory shock. New England Journal of Medicine, 369, 1726-3417.
- Vincent, J. L. (2011). Let’s give some fluid and see what happens” versus the “mini-fluid challenge. Anesthesiology, 115(3), 455–456.
- Bennett, V. A., Vidouris, A., & Cecconi, M. (2018). Effects of fluids on the macro- and microcirculations. Critical Care, 22(1), 74.
- Malbrain, M. L. N. G. et al. (2024). Rational Use of Intravenous Fluids in Critically Ill Patients. Springer Nature, 598.
- Cordemans, C. et al. (2012). Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak, and fluid balance. Annals of Intensive Care, 2(Suppl 1), S1.
- Malbrain, M. L. N. G. et al. (2018). Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Annals of Intensive Care, 8, 1-16.
- Annane, D. et al. (2013). Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA, 310(17), 1809–1817.
- Myburgh, J. A. et al. (2012). Hydroxyethyl starch or saline for fluid resuscitation in intensive care. New England Journal of Medicine, 367(20), 1901–1911.
- Нагайчук, В. І. et al. (2023). Перші результати міжнародного багатоцентрового клінічного дослідження RheoSTAT-CP0669 щодо ефективності та безпеки інфузійного розчину Реосорбілакт® у комплексному лікуванні пацієнтів з опіковою хворобою. INFUSION & CHEMOTHERAPY, 4, 5-12.
- Шаріпова, В. Х. et al. (2022). Перші результати міжнародного багатоцентрового клінічного дослідження RheoSTAT-CP0620 щодо ефективності та безпеки інфузійного розчину Реосорбілакт® у комплексній терапії сепсису. INFUSION & CHEMOTHERAPY, 2, 11-20.
- Фещенко, Ю. І. et al. (2021). Перші дані міжнародного багатоцентрового клінічного дослідження RheoSTAT-CP0698 щодо ефективності та безпеки інфузійного розчину Реосорбілакт® у комплексній терапії пневмонії. Пульмонологія, 5(498), 18-21.
- Kovalenko, O. M. (2019). Лікування опікового шоку на спеціалізованому етапі. The Ukrainian Journal of Clinical Surgery, 86(8), 55-58.
- Hypertonic saline resuscitation of hemorrhagic shock diminishes neutrophil rolling and adherence to endothelium and reduces in vivo vascular leakage
- urgent.com.ua/ua/archive/2018/1%2870%29/pages-5-13/oglyad-ievropeyskoyi-nastanovi-z-likuvannya-masivnih-krovotech-ta-koagulopatiy-pislya-travmi
- nlm.nih.gov/pmc/articles/PMC10161024/