Endothellitis as an important factor of Long Covid and ways of medical correction
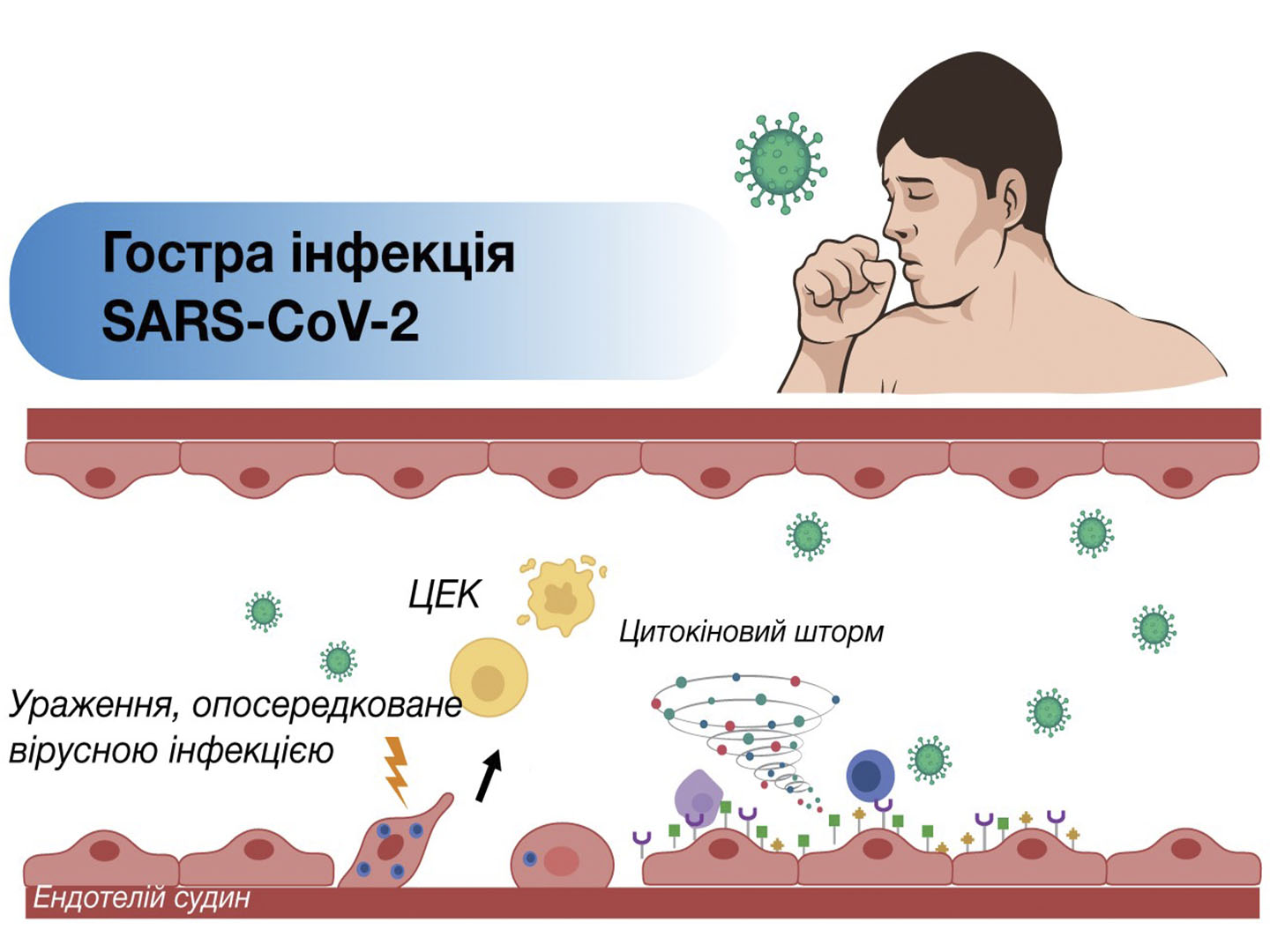
Abstract. COVID-19 coronavirus disease, which has become an unprecedented global challenge, is caused by a pro-inflammatory and prothrombogenic pathogen – coronavirus 2 (SARS-CoV-2), infection of which leads to the development of severe acute respiratory syndrome [López Castro, 2020; Higgins et al, 2021; Østergaard, 2021].
As of January 14, 2022, more than 318 million cases of COVID-19 have been confirmed; more than 5.5 million people have died from the disease [WHO, 2021].
The aim of the research is to systematize and generalize modern scientific data of evidence-based medicine on the features of Long COVID-syndrome and the role of endothelial dysfunction in its development.
The article presents modern scientific data of evidence-based medicine on Long COVID-syndrome and the importance of endothelium in its course.
Keywords: postcoid syndrome, Long COVID, endothelium, L-arginine, L-carnitine.
Author: Netyazhenko Vasyl Zakharovych, MD, Professor, Corresponding Member of the National Academy of Medical Sciences of Ukraine, Head of the Department of Propaedeutics of Internal Medicine № 1 of the National Medical University named after O.O. Bogomolets.
Literature:
- Ackermann M, Verleden SE, Kuehnel M, et al. . Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med2020; 383: 120–128.
- Aso K, Nishigawa T, Nagamachi S, Takakura M, Furuse M. Orally administrated D-arginine exhibits higher enrichment in the brain and milk than L-arginine in ICR mice. J Vet Med Sci. 2020 Mar 5;82(3):307-313. doi: 10.1292/jvms.19-0630
- Bahadoran Z, Mirmiran P, Tahmasebinejad Z, Azizi F. Dietary L-arginine intake and the incidence of coronary heart disease: Tehran lipid and glucose study. Nutr Metab (Lond). 2016 Mar 15;13:23. doi: 10.1186/s12986-016-0084-z.
- Bernard I, Limonta D, Mahal LK, Hobman TC. Endothelium Infection and Dysregulation by SARS-CoV-2: Evidence and Caveats in COVID-19. Viruses. 2021; 13(1):29. https://doi.org/10.3390/v13010029
- Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, Dentali F, Montecucco F, Massberg S, Levi M, Abbate A (2021). Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 21(5), 319-329
- Callard F, Perego E. How and why patients made Long Covid. Soc Sci Med. 2021 Jan;268:113426. doi: 10.1016/j.socscimed.2020.113426
- Carfì A, Bernabei R, Landi F; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020 Aug 11;324(6):603-605. doi: 10.1001/jama.2020.12603
- Chioh FW, Fong SW, Young BE, Wu KX, Siau A, Krishnan S, Chan YH, Carissimo G, Teo LL, Gao F, Tan RS, Zhong L, Koh AS, Tan SY, Tambyah PA, Renia L, Ng LF, Lye DC, Cheung C. Convalescent COVID-19 patients are susceptible to endothelial dysfunction due to persistent immune activation. Elife. 2021 Mar 23;10:e64909. doi: 10.7554/eLife.64909
- COVID-19 Symptom Study App, 2020. How Long Does COVID-19 Last-. Доступ: 14 вересня 2021. https://covid.joinzoe.com/post/covid-long-term.
- Cumpstey AF, Clark AD, Santolini J, Jackson AA, Feelisch M. COVID-19: A Redox Disease-What a Stress Pandemic Can Teach Us About Resilience and What We May Learn from the Reactive Species Interactome About Its Treatment. Antioxid Redox Signal. 2021 Jun 29. doi: 10.1089/ars.2021.0017.
- Deer R.R., Rock M.A., Vasilevsky N. et al. (2021) Characterizing Long COVID: Deep Phenotype of a Complex Condition. medRxiv, June 29. doi.org/10.1101/2021.06.23.21259416.
- Doykov I, Hällqvist J, Gilmour KC, Grandjean L, Mills K, Heywood WE. ‘The long tail of Covid-19’ – The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Res. 2020 Nov 19;9:1349. doi: 10.12688/f1000research.27287.2
- Fogarty H, Townsend L, Morrin H, Ahmad A, Comerford C, Karampini E, et al. Persistent endotheliopathy in the pathogenesis of long COVID syndrome. J Thromb Haemost. 2021 Aug 10:10.1111/jth.15490. doi: 10.1111/jth.15490
- Gambardella J, Khondkar W, Morelli MB, Wang X, Santulli G, Trimarco V. Arginine and Endothelial Function. Biomedicines. 2020 Aug 6;8(8):277. doi: 10.3390/biomedicines8080277.
- Guzik TJ, Mohiddin SA, Dimarco A, et al. . COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res2020; in press [10.1093/cvr/cvaa106].
- Hamilos M, Petousis S, Parthenakis F. (2018) Interaction between platelets and endothelium: from pathophysiology to new therapeutic options. Cardiovasc Diagn Ther. 8(5), 568-580
- Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol2004; 203: 631–637. doi:10.1002/path.1570
- Higgins V, Sohaei D, Diamandis EP, Prassas I. COVID-19: from an acute to chronic disease- Potential long-term health consequences. Crit Rev Clin Lab Sci. 2021 Aug;58(5):297-310. doi: 10.1080/10408363.2020.1860895
- Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Li Y, Xie W, Cui D, Shang L, Fan G, Xu J, Wang G, Wang Y, Zhong J, Wang C, Wang J, Zhang D, Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021 Jan 16;397(10270):220-232. doi: 10.1016/S0140-6736(20)32656-
- Huertas A, Guignabert C, Barbera JA, et al. . Pulmonary vascular endothelium: the orchestra conductor in respiratory diseases: highlights from basic research to therapy. Eur Respir J2018; 51: 1700745. doi:10.1183/13993003.00745-2017
- Huertas A, Montani D, Savale L, Pichon J, Tu L, Parent F, Guignabert C, Humbert M. Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)? Eur Respir J. 2020 Jul 30;56(1):2001634. doi: 10.1183/13993003.01634-2020
- Komaroff A.. The tragedy of the post-COVID “long haulers”. March 01, 2021. https://www.health.harvard.edu/blog/the-tragedy-of-the-post-covid-long-haulers-2020101521173
- Kumar A, Narayan RK, Kumari C, Faiq MA, Kulandhasamy M, Kant K, Pareek V. SARS-CoV-2 cell entry receptor ACE2 mediated endothelial dysfunction leads to vascular thrombosis in COVID-19 patients. Med Hypotheses. 2020 Dec;145:110320. doi: 10.1016/j.mehy.2020.110320
- Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, Greenhalgh T. Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv Res. 2020 Dec 20;20(1):1144. doi: 10.1186/s12913-020-06001-y
- Logue JK, Franko NM, McCulloch DJ, McDonald D, Magedson A, Wolf CR, Chu HY. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw Open. 2021 Feb 1;4(2):e210830. doi: 10.1001/jamanetworkopen.2021.0830. Erratum in: JAMA Netw Open. 2021 Mar 1;4(3):e214572
- López Castro J. Post-COVID-19 Syndrome (PC19S): Chronic Reactive Endotheliitis and Disseminated Vascular Disease. Acta Med Port. 2020 Dec 2;33(12):859. doi: 10.20344/amp.14612
- Luiking Y.C., Ten Have G.A., Wolfe R.R., Deutz N.E. Arginine de novo and nitric oxide production in disease states. J. Physiol. Endocrinol. Metab. 2012;303:E1177–E1189. doi: 10.1152/ajpendo.00284.2012
- Luther JM, Gainer JV, Murphey LJ, et al. . Angiotensin II induces interleukin-6 in humans through a mineralocorticoid receptor-dependent mechanism. Hypertension2006; 48: 1050–1057. doi:10.1161/01.HYP.0000248135.97380.76
- McFadyen JD, Stevens H, Peter K. The Emerging Threat of (Micro)Thrombosis in COVID-19 and Its Therapeutic Implications. Circ Res. 2020 Jul 31;127(4):571-587. doi: 10.1161/CIRCRESAHA.120.317447.
- Mehta P, McAuley DF, Brown M, et al. . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet2020; 395: 1033–1034. doi:10.1016/S0140-6736(20)30628-0
- Merrill, J.T., Erkan, D., Winakur, J. et al.Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol 16, 581–589 (2020). https://doi.org/10.1038/s41584-020-0474-5
- Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: Consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep. 2021 Feb;9(3):e14726. doi: 10.14814/phy2.14726
- Pagano G, Manfredi C, Pallardó FV, Lyakhovich A, Tiano L, Trifuoggi M. Potential roles of mitochondrial cofactors in the adjuvant mitigation of proinflammatory acute infections, as in the case of sepsis and COVID-19 pneumonia. Inflamm Res. 2021 Feb;70(2):159-170. doi: 10.1007/s00011-020-01423-0
- Pober JS, Sessa WC (2007). Evolving functions of endothelial cells in inflammation. Nat Rev Immunol. 7(10), 803-15.
- Silva Andrade B, Siqueira S, de Assis Soares WR, de Souza Rangel F, Santos NO, Dos Santos Freitas A, Ribeiro da Silveira P, Tiwari S, Alzahrani KJ, Góes-Neto A, Azevedo V, Ghosh P, Barh D. Long-COVID and Post-COVID Health Complications: An Up-to-Date Review on Clinical Conditions and Their Possible Molecular Mechanisms. Viruses. 2021 Apr 18;13(4):700. doi: 10.3390/v13040700
- Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021 Apr;27(4):626-631. doi: 10.1038/s41591-021-01292-y.
- Thakkar S., Arora S., Kumar A. et al. (2020) A Systematic Review of the Cardiovascular Manifestations and Outcomes in the Setting of Coronavirus-19 Disease. Clin. Med. Insights. Cardiol.; 14: 1179546820977196
- WHO, 2021. Coronavirus disease (COVID-19) pandemic https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Доступно 01-12-2021
- Wu G, Bazer FW, Davis TA, Kim SW, Li P, Marc Rhoads J, Carey Satterfield M, Smith SB, Spencer TE, Yin Y. Arginine metabolism and nutrition in growth, health and disease. Amino Acids. 2009 May;37(1):153-68. doi: 10.1007/s00726-008-0210-y.
- Zahran AM, El-Badawy O, Ali WA, Mahran ZG, Mahran EEMO, Rayan A (2021). Circulating microparticles and activated platelets as novel prognostic biomarkers in COVID-19; relation to cancer. PLoS One. 2021 Feb 22;16(2):e0246806.
- Zhang W., Zhao Y., Zhang F. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The Perspectives of clinical immunologists from China. Clinical Immunology. 2020; 214: 108393.
- Ziegler CGK, Allon SJ, Nyquist SK, et al. . SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell2020; 181: 1016–1035. doi:10.1016/j.cell.2020.04.035
- Галушко О.А. Астенічний синдром у постковідного пацієнта. Медична газета «Здоров’я України 21 століття» №6 (499), 2021 р.
- Коваленко С.В. Досвід застосування методів синдромно-патогенетич¬ної терапії при пневмонії, спричиненій COVID-19, в умовах пульмоно¬логічного відділення. Медична газета «Здоров’я України 21 сторіччя» № 13-14 (481-482), 2020 р.
- Курята, М. М. Гречаник. Роль L-аргініну в лікуванні серцево-судинних захворювань: у фокусі – вибір ефективної дози. О.В. Медична газета “Здоров’я України”, No11 (456), 2019 р.
- Матюха Л.Ф. «Далекобійники»: пацієнти з постковідним синдромом у рутинній клінічній практиці. Журнал «Здоров’я України» №4, 2021.