Clinical-biochemical rationale of use of Mannitol and Sorbilact in severe craniocerebral injury
Danylo Halytsky Lviv National Medical University
Severe craniocerebral injury is accompanied by focal and cerebral symptoms associated with the damage to certain sections of the brain, its perifocal edema, endoge-nous intoxication (1,8).
In the initial stages, edema and swelling of the brain are a protective reaction in response to the damage as hy-perhydration reduces the concentration of toxins in cells of the brain. However, the progression of the process leads to a dramatic increase in the intracranial pressure and de-velopment of dislocation phenomena that affect the stem sections of the brain that may cause disruption of the vital functions and be responsible for the death of a patient (10).
It is clinically represented with impairment of con-sciousness, as evidenced by decreasing Glasgow coma scale (< 9 points) and symptoms of brain structure dislo-cation. In these cases, osmotic diuretics are widely used: mannitol, sorbitol, glycerol and saluretic furosemide and, recently, domestic osmotic diuretics of polyfunctional ac-tion Sorbilact and Rheosorbilact (4,7).
The first phase of action of diuretics is characterized by a rapid (within 15–30 min) decrease in the intracranial pressure. In this period, the intratissue pressure is reduced in those parts of the brain where the vascular regulation and blood-brain barrier (BBB) permeability are not af-fected, whereas the intratissue pressure in the parts of the brain with affected BBB may increase by 10–25%. The second phase (30–90 min after osmotic diuretics admin-istration) is characterized by the maximum drop of the cer-ebrospinal fluid pressure (up to 50%) and intratissue pres-sure (88%), accompanied by an increase in cerebral blood flow by 20–40%. In the third phase (2.5 – 3.5 hours after the drug administration), with occurrence of “rebound syn-drome” in 65% of cases, the CSF pressure and intratissue pressure exceed the initial values. Diuretics are also pre-scribed as a therapeutic measure aimed at treating endo-toxicosis (8).
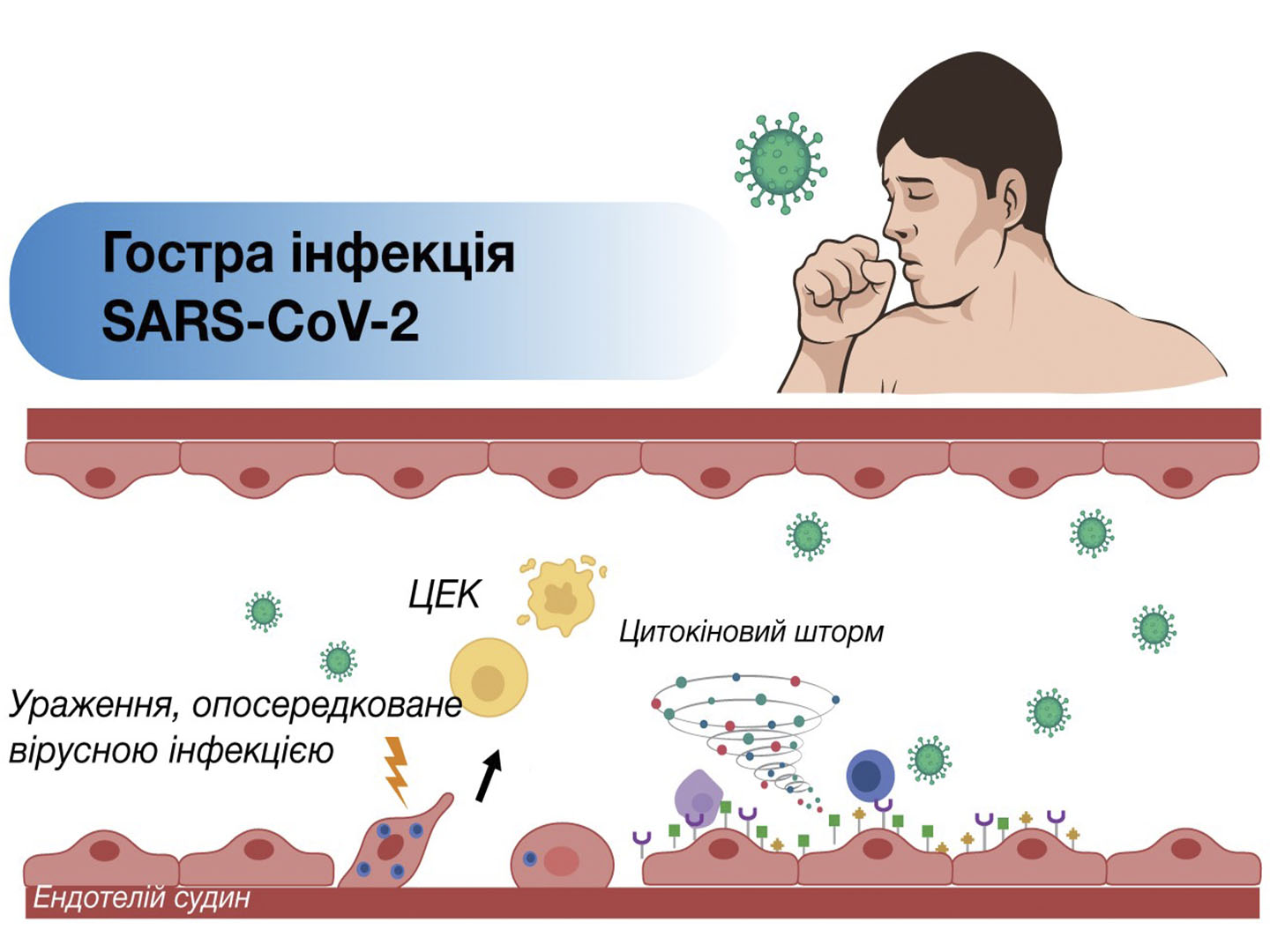
In craniocerebral injury (CCI), it is associated with de-struction of the brain tissue, blood vessel ruptures, en-trance of macro- and micro-parts of cerebral detritus into the blood flow, direct contact of poured out blood with the brain tissue, formation of intracranial hematoma, blood in-filtration in the cerebrospinal fluid.
Since in CCI the function of the blood-brain barrier is disturbed and the permeability of capillaries increases, their epithelium is damaged, a significant mass of frag-ments of the damaged tissue moves from the brain to the general circulation, which causes endogenous intoxication (EI) (8). In this regard, the detoxification therapy is one of the components of the treatment of severe CCI. It involves elimination of toxins from various fluid media of the body (blood, plasma, lymph, cerebrospinal fluid) (9).
Detoxification therapy is conducted for activation and optimization of the physiological systems of the body re-sponsible for elimination of toxins. The main principles of detoxification are:
⋅ enhancing perfusion in order to create conditions for the diffusion of toxic factors from affected cells, tis-sues into the general circulation;
⋅ haemodilution that results in decreased plasma con-centration of toxins;
⋅ forced diuresis resulting in faster excretion of toxins and metabolites from the body. With this purpose, di-uretics are most often used.
Priority is given to osmotic diuretics since their action starts faster and is more physiological than that of saluret-ics. Effect of osmotic diuretics is manifested not only in the reduction of brain edema and intracranial pressure, but also in improvement of the rheological properties of blood, cerebral blood flow and, unlike saluretics, when osmotic diuretics are used, hypovolaemia and hyponatraemia are more rarely observed.
Mannitol reduces intracranial pressure by 15–20%, im-proves the cerebral perfusion pressure by 10%, increases cerebral blood flow by 10–15% and stimulates increase in its flow rate by 13%. Unlike furosemide, mannitol improves the rheological properties of blood: reduces its viscosity by 16% (furosemide increases by 25%), reduces the haema-tocrit by 37% (furosemide – increases by 2%), does not affect the aggregation of platelets (furosemide increases by 20%). (2,3). The disadvantages of mannitol, especially furosemide, include the ability to cause a “rebound syn-drome”, blood electrolyte disturbance. These disad-vantages can be reduced by administration of Sorbilact and Rheosorbilact that have the necessary electrolytes (potassium, sodium, magnesium, chlorine) in their compo-sition in balanced proportions (4.6.7).
According to M.E. Polishchuk (2002), these drug prod-ucts have a diuretic effect, significantly improve the func-tion of the kidneys and liver, stimulate intestinal peristalsis, optimize hemodynamics in traumatic and hemorrhagic shock, which makes their widespread use in severe brain injuries justified.
A statement made by a competitive company about the possibility of complications when using large doses of sor-bitol, as well as the work by E.I. Bulss, H.I. Van Zuylen (1997) about the risk of hyperglycemia, hypophosphatae-mia and lactatemia in these cases has caused the need to study the impact of the recommended by the releaser doses of Sorbilact and Rheosorbilact on the frequency of complications and on the level of glycemia, lactatemia, in-organic phosphate blood levels in patients with severe craniocerebral injury. For this purpose, data on the use of more than 1 million bottles of Sorbilact and Rheosorbilact in Ukraine were analyzed. It was found that there were no claims to the company in connection with the complica-tions. The task of the work was to study the impact of these drug products on the level of glucose, inorganic phosphate, lactate and endotoxicosis values.